Scientists in many fields received little recognition for the last
couple of years, as the world focused on the emergency push to develop
vaccines and treatments for Covid-19. But that doesn't mean they weren't
still busy researching a dizzying series of developments that are now
being reported as major discoveries and achievements.
1. First pig kidney transplant
Scientists
successfully transplanted a pig's kidney into a human. If the organ
takes successfully, it could be a game-changer for those waiting in vain
on the kidney transplant list. "I saw it not only as a way to help me,
but a way to provide hope for the thousands of people who need a
transplant to survive," said Richard Slayman, who received the
transplant, to The Associated Press. The surgery took four hours and 15 people to execute.
Pigs
have long been used in medicine for procedures like skin grafts and
implantations of heart valves. However, "transplanting entire organs is
much more complex than using highly processed tissue," said the AP,
adding that the pig was "genetically edited to remove harmful pig genes
and add certain human genes to improve its compatibility." Slayman now
needs to be monitored for any rejection of the kidney. "He would have
had to wait five to six years for a human kidney. He would not have been
able to survive it," Dr. Winfred Williams, an associate chief of the
nephrology division at Mass General, said to The New York Times.
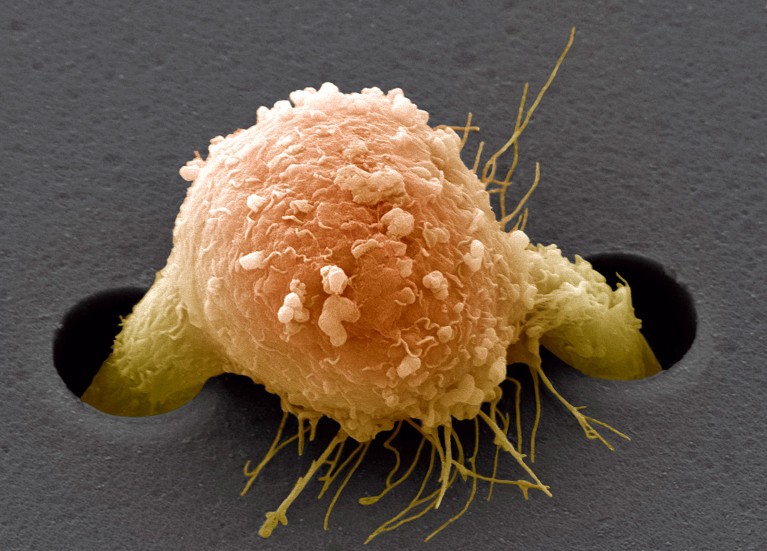
2. Cell therapy for melanoma
The
U.S. Food and Drug Administration (FDA) approved the first cellular
therapy for aggressive forms of melanoma. The treatment, called Amtagvi,
is "designed to fight off advanced forms of melanoma by extracting and
replicating T cells derived from a patient's tumor," said
NPR.
These cells are also called tumor-infiltrating lymphocytes (TIL). T
cells are integral in the immune system but can become "dysfunctional
inside tumors.
"The approval of Amtagvi
represents the culmination of scientific and clinical research efforts
leading to a novel T cell immunotherapy for patients with limited
treatment options," Dr. Peter Marks, the director of the FDA's Center
for Biologics Evaluation and Research, said in a statement.
The treatment won't work for everyone, but research by the National
Institutes of Health showed a "56% response rate among patients with
melanoma, and 24% of patients had a complete disappearance of their
melanoma, regardless of where it was," Axios
said. "This is the tip of the iceberg of what TIL can bring to the
future of medicine," Patrick Hwu, CEO of Moffitt Cancer Center, said to Axios.
3. Rhino IVF
Scientists
were able to impregnate a southern white rhino using in-vitro
fertilization (IVF). Researchers in Kenya implanted a southern white
rhino embryo into another of the same species using the technique in
September 2023, resulting in a successful pregnancy. The technique could
be used to save the northern white rhino from total extinction. "We
achieved together something which was not believed to be possible," Thomas Hildebrandt,
head of the reproduction management department at the Leibniz Institute
for Zoo and Wildlife Research, said in a press conference.
There
are two species of white rhinos: northern and southern. The northern
white rhino is on the verge of extinction due to poaching, with only two
females remaining. Luckily, scientists have sperm preserved from the
last male rhino, which could be combined with an egg from the female and
implanted into a southern white rhino female to act as a surrogate.
Using a white rhino embryo to test the procedure was a "proof of
concept" which is a "milestone to allow us to produce northern white
rhino calves in the next two, two and a half years," Hildebrandt said.
4. Pristine configuration
Scientists
discovered six exoplanets that revolve around a star in a rare pattern
called orbital resonance, said a study published in the journal Nature.
This means that "for every six orbits completed by planet b, the
closest planet to the star, the outermost planet g completes one," CNN
said, adding that "as planet c makes three revolutions around the star,
planet d does two, and when planet e completes four orbits, planet f
does three."
The system was
deemed a "rare fossil" by Rafael Luque, a postdoctoral scholar in the
University of Chicago's Department of Astronomy and Astrophysics. "We
think only about one percent of all systems stay in resonance," Luque
said in a statement.
"It shows us the pristine configuration of a planetary system that has
survived untouched." The discovery could help further the study of
sub-Neptunes, which are planets larger than Earth but smaller than
Neptune. They are not present in our solar system. "There is little
agreement among astronomers about how these planets form and what
they're made of — so an entire system consisting of sub-Neptunes could
help scientists determine more about their origin," Luque said.
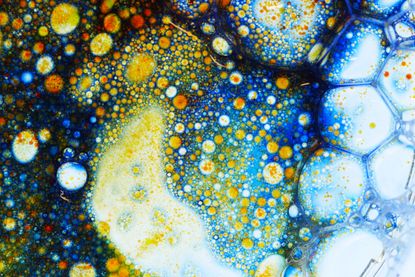
5. Restoring reefs
Coral bleaching has been a rapidly growing problem
as climate change worsens. Without intervention, the reefs will
continue to deteriorate. To counter this, scientists have explored the
idea of a "coral gym," essentially a "laboratory to make corals
stronger," NPR said. The goal is to "train" coral to survive more extreme conditions.
Warming oceans
and rising temperatures are the largest contributors to coral
degradation. "One of the things that we do in this lab is subject them
to different environmental conditions and evaluate who's a little bit
stronger," Ian Enochs, lead of the Coral Program at the Atlantic
Oceanographic and Meteorological Laboratory at the National Oceanic and
Atmospheric Administration, said to NPR. Researchers created a "complex
matrix of aquariums" where they can "subject different types of corals
to different environments and not only understand how they might
survive, but perhaps help them to do so."
6. AI to find aliens
Scientists have created an artificial intelligence model that can detect alien life, said a study published in the journal PNAS.
The algorithm can "distinguish between samples of biological and
nonbiological origin 90% of the time," after being "trained using living
cells, fossils, meteorites and lab-made chemicals," Live Science
said. "Put another way, the method should be able to detect alien
biochemistries, as well as Earth life," Robert Hazen, co-author of the
study, said in a statement.
The AI "does not involve a machine having to look for specific things," but rather "looks for differences between samples," BBC
said. "These results mean that we may be able to find a lifeform from
another planet, another biosphere, even if it is very different from the
life we know on Earth," Hazen continued. "And, if we do find signs of
life elsewhere, we can tell if life on Earth and other planets derived
from a common or different origin."
7. Inverse vaccines
Scientists may have found a way to calm immune responses for those with autoimmune disorders using an "inverse vaccine," said a study published in the journal Nature Biomedical Engineering.
The immune system responds to specific identifying markers on invaders
like viruses and bacteria called antigens, "but some immune cells react
to self-antigens," which are "molecules from our own cells," said Science. "In autoimmune diseases, these misguided immune cells turn against patients' own tissues."
The
new research worked by "directing potential self-antigens to the
liver," where "immune cells there pick up self-antigens and then stifle T
cells that could target these molecules." The experiment was performed
on mice. "The method they use is promising and potentially can induce
better tolerance," neurologist and neuroimmunologist A.M. Rostami said
to Science, adding that "we don't know" whether this approach is
"applicable to human disease in which we don't know the antigen."
8. Sequencing the Y-chromosome
Scientists
have finally sequenced the entire Y chromosome, one of the human sex
chromosomes present in those assigned male at birth. The feat has been
"notoriously difficult" because of the Y chromosome's "complex repeat
structure," said a research paper published in the journal Nature.
"Just
a few years ago, half of the human Y chromosome was missing" from
knowledge of the human genome, Monika Cechova, co-lead author on the
paper, said to CNN.
"I would credit new sequencing technologies and computational methods
for this," Arang Rhie, who also worked on the paper, said to Reuters. The X chromosome was fully sequenced back in 2020.
Understanding
the Y chromosome can help with a number of health issues, including
fertility. Genes have also "been shown to be required for the prevention
of cancer and cardiovascular disease," Kenneth Walsh, a professor of
biochemistry and molecular genetics at the University of Virginia School
of Medicine, said to CNN.
9. Discovering the motion of space-time
Scientists found evidence that the fabric of space and time gets warped by gravitational waves. "What we measure is the Earth kind of moving in this sea," astrophysicist Michael Lam said to The Washington Post.
"It's bobbing around — and it's not just bobbing up and down, it's
bobbing in all directions." The findings affirm a facet of Einstein's
Theory of Relativity that "space is not serenely empty, and time does
not march smoothly forward," the Post said.
What
scientists discovered was the "low-pitch hum of gravitational waves
resounding throughout the universe," and the findings were published in The Astrophysical Journal Letters.
While the cause of the hum is not certain, scientists believe it
originated from supermassive black holes circling each other, said The Wall Street Journal.
"Before now, we didn't even know if supermassive black holes merged,
and now we have evidence that hundreds of thousands of them are
merging," said Chiara Mingarelli, a Yale University astrophysicist and a
member of the North American Nanohertz Observatory for Gravitational
Waves (NANOGrav), which led the research, to the Journal.
The
gravitational wave finding "does not put any torque on everyday human
existence," said the Post, "but it does offer potential insight into the
physical reality we all inhabit."
10. Gene therapy for muscular dystrophy
The Food and Drug Administration approved gene therapy for children with Duchenne muscular dystrophy, said NPR. The treatment is limited to children aged four and five while more research is being done on its safety and effectiveness.
Muscular
dystrophy appears in boys far more often than girls and can be
debilitating, or even fatal in a person's 30s or 40s. The treatment,
developed by Sarepta Therapeutics, has faced some criticism, as there
are some concerns about whether it is actually safe and effective.
11. Improving heart health
A
daily pill, bempedoic acid, has proved its ability to reduce the risk
of heart disease, especially in those who have adverse reactions to
statins, said a study published in the New England Journal of Medicine.
Statins are normally prescribed to reduce cholesterol; however, many
individuals cannot take them or choose not to take them because of side
effects. "Statins are known to cause muscle aches in a subset of
people," said USA Today.
Bempedoic
acid works similarly to statins, but since it is only activated in the
liver, is less likely to cause muscle aches. Side effects include an
increased risk of gout.
12. AI mind reading
Scientists
have created an AI-based decoder that can turn a person's brain
activity into text, said a paper published in the journal Nature. The system is non-invasive, meaning it doesn't require any surgical implants, and uses the same AI technology as chatbot ChatGPT. The technology scanned brain activity and predicted what words a person was listening to.
"We don't like to use the term mind reading," Alexander Huth, who worked on the research, said to CNN.
"We think it conjures up things that we're actually not capable of." He
said the "real potential application of this is in helping people who
are unable to communicate." To allay any concerns about whether the
technology could pose a threat to privacy once further developed, Jerry
Tang, the lead author of the paper, said everyone's brain data should be private. "Our brains are kind of one of the final frontiers of our privacy."
13. Slowing Alzheimer's
A
drug from pharmaceutical company Eli Lilly showed signs of slowing the
advance of Alzheimer's disease by approximately one-third, BBC
said. The drug, called donanemab, acts as an antibody specifically
created to attack and remove "sticky gunk" called beta-amyloid, which
"builds up in the spaces between brain cells, forming distinctive
plaques that are one of the hallmarks of Alzheimer's," BBC said. "We are
now entering the time of disease modification, where we might
realistically hope to treat and maintain someone with Alzheimer's
disease, with long-term disease management rather than palliative and
supportive care," Dr. Cath Mummery of the U.K.'s National Hospital for
Neurology and Neurosurgery said to the outlet.
A side effect, however, is fatal swelling in the brain, which potentially affected three of the clinical trial participants.